CLINICAL INDICATIONS & BENEFITS OF IN-HOUSE DIAGNOSTIC TESTING
CLINICAL INDICATIONS
Common clinical indications for testing:
- Carpal Tunnel Syndrome
- Causalgia
- Cord Trauma
- Disc Disease
- Disc Disease Syndrome
- Generalized Arterial Wall Disease
- Hyperflexion/Extension Injury
- Malingering
- Nerve Entrapment/Neuropathy
- Nerve Root Irritation
- Neuritis/Sensory Deficits
- Peripheral Nerve Trauma
- Plexis Stretch Injury
- Radiculitis
- Sensory Dysfunction
- Sciatica/Radicular Pain
- Spinal Stenosis
- Systemic Neuropathies
- Tarsal Tunnel Syndrome
- Thoracic Outlet Syndrome
- Vertebral Subluxation Complex
BENEFITS OF IN-HOUSE DIAGNOSTIC TESTING
Take advantage of the many benefits that In-House Diagnostic Testing Offers You and Your Patients:
- Convenient in-house diagnostic testing
- Objective documentation from Board Certified Physicians
- Professional on-staff technicians and support team
- Efficient, convenient and timely scheduling, based on your needs
- Insurance authorization performed through SNG staffBilling and reimbursement assistance
- Substantiation of extended care
NERVE STUDIES
Diagnostic focus is on radiculopathies, neuropathies, demylination of the nerve and axonal loss.
The motor and sensory components of the nerve are evaluated.
The nerve study consists of a Nerve Conduction Velocity (NCV), F-Wave/H-Reflex and Dermatomal
Somatosensory Evoked Potential (DSEP) tests. Integrity of the nerve is diagnosed by the following criteria:
To obtain a complete picture of the patient’s problem areas, both motor and sensory components of the nerve are tested.
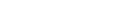
NERVE CONDUCTION VELOCITY(NCV), F-WAVE AND H-REFLEX
Nerve Conduction Velocity (NCV) is used to measure action potentials resulting from peripheral nerve stimulation. The reaction times (latencies) and velocities obtained will detect neurological problems or compression of the nerves throughout the extremity. The F-Wave looks at the most proximal segment of the nerve, including the root. The reaction time (latency) will show if there is a delay at the spinal level of the particular nerve.
The Tibial H-Reflex is considered to reflect that state of the S1 nerve root and its sensory component. Collectively, the F-Wave and H-Reflex look at compression at the cord level.
By testing both the motor and sensory components of the nerve, a doctor can garnish a comprehensive picture of the patient’s problem areas.
“The clinical utility of Nerve Conduction Velocities (NCV) is based upon its ability to: 1) demonstrate abnormal sensory function when the history and/or neurological examination are equivocal; 2) reveal the presence of clinically unsuspected malfunction in a sensory system, when demyelinating disease is suspected because of symptoms and/or signs in another area of the Central nervous System (CNS); 3) help define the anatomic distribution of a disease process; and 4) monitor objective changes in a patient’s status.
These tests provide reproducible, sensitive, quantitative extensions of the clinical neurological examination…NCV’s are essential to the modern practice of medicine because they: 1) provide data unobtainable without the use of amplifiers and oscilloscopes; 2) quantify and objectify data which the clinician may sense; 3) localize lesions within a long sensory pathway; 4) are more efficient and cost-effective because the testing is done by paramedical personnel who can be trained more expeditiously than neurologists, ophthalmologists and otolaryngologists.”
K. Chiappa, M.D., Evoked Potential in Clinical Medicine, 1990 (condensed and reprinted).
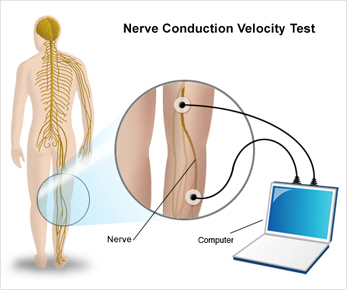
DERMATOMAL SOMATOSENSORY EVOKED POTENTIAL (DSEP)
 Dermatomal Somatosensory Evoked Potential (DSEP) involves mild stimulation of the dermatomal region and records the reaction time to the cortex. DSEP looks for nerve root compression.
Dermatomal Somatosensory Evoked Potential (DSEP) involves mild stimulation of the dermatomal region and records the reaction time to the cortex. DSEP looks for nerve root compression.
“For most neurological problems, two issues addressed by somatosensory evoked potentials (SEPs) are the verification of a conduction abnormality and the localization of that abnormality along the neuroaxis. Conventional SEPs to mixed nerves stimulation may adequately verify a conduction abnormality, but not its location. From a technical standpoint, DSEPs are easier to record than Spinal SEPs and could serve as a useful technique for localization of neurological abnormalities along the neuroaxis.”
Jefferson C. Slimp, PhD, et al, “Dermatomal somatosensory evoked potentials: Cervical, thoracic and lumbosacral levels.” Electroencephalography and Clinical Neurophysiology.
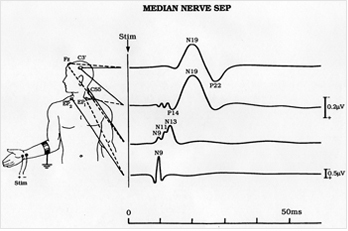
ELECTROMYOGRAPHY (EMG)
In some states, Needle Electromyography (EMG) is offered in conjunction with the nerve study. Electromyography tests the integrity of the entire motor system, which consists of upper and lower motor neurons, the neuromuscular junction and muscle. It is an invasive technique that requires needle insertion and adjustment at multiple sites. Activation of the motor unit will cause a potential wave form from the recording needle, as well as audible sound, which is also diagnostic. Depending on our findings, at least five muscles will be tested that correlate with the specific nerve distribution of the affected area.
Electromyography (EMG) studies the intrinsic electrical properties of skeletal muscles. Electromyography is offered only in certain states.
DIAGNOSTIC SPINAL ULTRASOUNDS
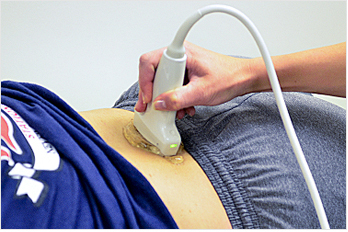
Diagnostic focus is on the facet, muscle and ligament of the vertebral and paravertebral region for
inflammation due to the patient’s injury.
- Upper exam consists of the Cervical Spine, T1-T6 and Trapezius muscles bilaterally
- Lower exam consists of T6-T12, Lumbar Spine and Sacroiliac joints bilaterally
- Full Series (Upper and Lower) exam can be ordered, if warranted.
Doctors frequently order a Nerve Study in conjunction with a Diagnostic Spinal Ultrasound for the effected area to correlate the findings.
Nerve Tests Should be Ordered When:
- Subjective complaints are evident, but objective findings are not supportive
- X-rays, CT or MRI are negative, yet symptoms persist
- Non-resolving radicular pain is present
- Nerve irritation or damage needs to be determined
- Evaluation and substantiation of continued care is required
- Real versus imagined pain must be assessed
About Diagnostic Spinal Ultrasonography
Diagnostic Spinal Sonography plays a valuable role as a differential diagnostic modality, allowing the physician to objectively identify soft tissue pathology. Its focus is on the facet, muscle and ligament of the vertebral and paravertebral region, isolating musculoskeletal trauma from the cystic or solid character of a swelling or mass. Diagnostic Ultrasound records changes to the soft tissue around each vertebra and aids in the subtreatment evaluation process.
This practical method of monitoring the treatment and recovery of patients with soft tissue abnormalities is well-accepted and poses no discomfort to the patient. The examination is performed quickly and easily, is 100% reproducible, uses no radiation and is performed with a minimum of patient preparation.
“Ultrasound has been available since 1912…further development has led to [its] ability to discern fine anatomical detail. Ultrasound is now employed in obstetrics, cardiology, nephrology and gastroenterology…Ultrasound is a valuable and cost-effective diagnostic modality. In pain management, its primary function is to diagnose lesions of soft musculoskeletal structures causing pain, otherwise not easily identified by conventional radiologic examinations.”
J. Antonio Aldrete, M.D., M.S., “Diagnostic Ultrasound in Pain Management: An Overview,” American Journal of Pain Management Electroencephalography.
Benefits of Diagnostic Spinal Ultrasonography
- Provides objective documentation of soft tissue injuries and subjective complaints
- Pinpoints the location of trauma
- Scans the spine for nerve and muscle irregularities
- Determines recent versus prior injury
- Presents baseline documentation of initial patient visit
- Monitors patient response to treatment
When Spinal Ultrasonography Tests Should be Ordered
- Patient begins treatment, or 7 to 10 days post-trauma, to establish a treatment plan and baseline pathology
- Patient does not respond to care as anticipated
- Patient has subjective pain complaints, but the objective findings do not support them
- Patient’s complaints persist despite negative X-rays, CT scans or MRIs
- Soft tissue irritation or drainage must be determined
- Objective findings are necessary (as in legal cases)
- Condition reassessment is required for supportive documentation for continuous treatment
VASCULAR TESTING
Diagnosing disorders of the arteries and veins in the upper and lower extremities.
- Upper exam includes evaluation of the vessels of the arm. The arterial exam comprises of the Brachial, Radial and Ulnar arteries. The Venous exam includes the Subclavian, Axillary and Brachial veins. Comparison is made between the right and left arms, which are correlated to the clinical symptoms.
- Lower exam includes evaluation of the vessels of the legs. The arterial exam comprises of the Superficial Femoral, Posterior Tibial, and Popliteal arteries. The Venous exam includes the Common Femoral, Superficial Femoral and Popliteal veins. Comparison is made between the right and left legs, which are correlated to the clinical symptoms.
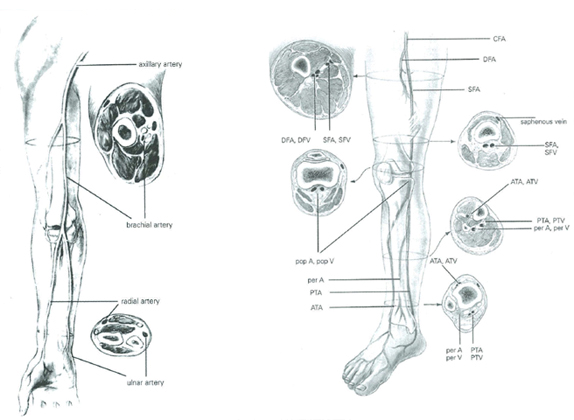 Vascular testing helps diagnose disorders of the arteries and veins in the legs, arms, neck and head utilizing non-invasive ultrasonic and imaging technologies. By measuring blood flow, these tests accurately document the presence, location and severity of occlusion. Occlusion occurs when plaque builds up in the arteries and veins that carry blood to and from the head, organs, and limbs. Plaque is made up of fat, cholesterol, calcium, fibrous tissue, and other substances in the blood. Over time, plaque can harden and narrow the arteries and veins, which limits the flow of oxygen-rich blood to and from the organs and other parts of the body. Early detection can be life saving and can help prevent serious conditions such as stroke and heart problems.
Vascular testing helps diagnose disorders of the arteries and veins in the legs, arms, neck and head utilizing non-invasive ultrasonic and imaging technologies. By measuring blood flow, these tests accurately document the presence, location and severity of occlusion. Occlusion occurs when plaque builds up in the arteries and veins that carry blood to and from the head, organs, and limbs. Plaque is made up of fat, cholesterol, calcium, fibrous tissue, and other substances in the blood. Over time, plaque can harden and narrow the arteries and veins, which limits the flow of oxygen-rich blood to and from the organs and other parts of the body. Early detection can be life saving and can help prevent serious conditions such as stroke and heart problems.Benefits of vascular testing:
- Prevent serious, life threatening conditions
- Reveal clots and other vascular-related disease
- Help form a customized treatment plan
- Utilizes tests that are painless and noninvasive
- Affordable methodology with quick results performed by trained technicians
Vascular testing should be ordered when:
- Patient has symptoms of vascular compromise
- History or family history of high blood pressure, stroke or heart disease
- X-ray findings of vertebral artery calcification
- Diagnosis of upper extremity nerve complaints
- Pain, numbness, tingling and swellings
- Signs of thoracic outlet syndrome
- Positive orthopedic tests for Adson’s, Halsted’s Eden’s, Wright’s, Allen’s